You are here
Prevention and Treatment of HIE
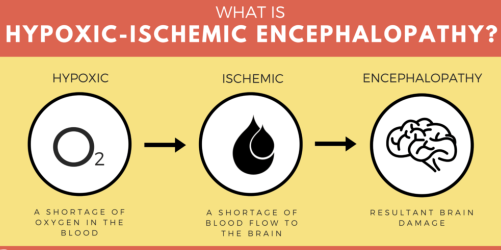 Hypoxic-ischemic encephalopathy (HIE) is a type of brain damage caused by an interruption in the flow of oxygenated blood to a baby’s brain around the time of birth. HIE can lead to serious conditions such as cerebral palsy, intellectual/developmental disabilities, speech and language disorders, epilepsy, hearing and vision limitations, and respiratory issues.
Hypoxic-ischemic encephalopathy (HIE) is a type of brain damage caused by an interruption in the flow of oxygenated blood to a baby’s brain around the time of birth. HIE can lead to serious conditions such as cerebral palsy, intellectual/developmental disabilities, speech and language disorders, epilepsy, hearing and vision limitations, and respiratory issues.
Although there are many treatments and therapies that can improve function in people with HIE and associated conditions, curative options are lacking. Stem cell therapy holds promise, but in the meantime, the only way to ensure that a baby will not experience the effects of HIE throughout their lifetime is to prevent oxygen deprivation from occurring in the first place.
The following measures can be very important in the prevention of HIE:
Prenatal Testing: There are certain tests that all expectant mothers should have in order to ensure that their babies are healthy and developing as they should. Women who have high-risk pregnancies (which may involve conditions such as preeclampsia, diabetes, or obesity) should receive more frequent and extensive prenatal testing. Common prenatal tests include non-stress tests, contraction stress tests, amniotic fluid volume tests, biophysical profiles, and Doppler velocimetry. If the results of any of these tests indicate that the baby is at risk for HIE, doctors may be able to intervene.
Preventing Premature Birth: Preterm babies are at high risk for HIE because they are still in the process of developing and have fragile organs. Their brains are especially vulnerable to brain bleeds and other injuries that can cause HIE. Therefore, if a woman has a history of preterm birth or other risk factors that indicate she may deliver prematurely, medical professionals should attempt to prevent the premature birth if possible. Common means of doing this include cervical cerclage and progesterone.
- Cervical cerclage is a stitch that is temporarily placed in the cervix and removed before a baby is ready to be born. Doctors often recommend that women with cervical insufficiency have a cerclage in order to stop the cervix from shortening or opening too early.
- Progesterone is a hormone that thickens the uterine lining to protect the growing baby and help avoid preterm delivery. Injections of progesterone have been used for more than 45 years to reduce preterm deliveries1, and are now available in an auto-injection formulation2.
 Minimizing the Risks Associated with Premature Birth: In addition to attempting to prevent preterm birth, physicians can minimize the risks associated with prematurity. Doctors often give pregnant women betamethasone and magnesium sulfate before a premature delivery.
Minimizing the Risks Associated with Premature Birth: In addition to attempting to prevent preterm birth, physicians can minimize the risks associated with prematurity. Doctors often give pregnant women betamethasone and magnesium sulfate before a premature delivery.
- Betamethasone is a corticosteroid that can help speed up lung development. It causes the release of surfactant, which lubricates the lungs so that they can slide against one another when the infant breathes. In general, full-term babies produce enough surfactant naturally, but premature infants may not. Betamethasone can reduce their risk of developing serious respiratory problems, HIE, and other complications.
- Magnesium sulfate is an inorganic salt, which can protect the fetal brain before premature birth. It can decrease the incidence and severity of HIE and cerebral palsy.
Proper Care During Delivery: During the birthing process, medical professionals must carefully monitor the mother and baby for signs of fetal distress, which indicate oxygen deprivation. Depending on the severity and cause of fetal distress, interventions may involve repositioning the mother, giving her oxygen and IV fluids, or performing an emergency C-section. Physicians must also follow other standards of care in delivery, and draw upon their extensive schooling and experience in order to manage any emergency situations that may arise.
C-Section Delivery: In some cases, a C-section delivery is needed in order to prevent HIE. If there is a known risk factor that would make vaginal delivery dangerous (such as preeclampsia or IUGR), a C-section will likely be scheduled in advance. If there is a less predictable or undiagnosed complication, an emergency C-section may be needed.
Interventions that can help babies with HIE:
The brain damage caused by hypoxic-ischemic injury is usually considered permanent, and most treatments for HIE are supportive in nature. Two treatments that can reduce the extent of damage caused by hypoxic-ischemic injury, and may be able to prevent serious lasting harm, are therapeutic hypothermia and stem cell therapy.
- Therapeutic Hypothermia involves cooling the baby’s brain down to a hypothermic temperature in order to allow brain cells to recover from injury and prevent further spread of damage. Multicenter clinical trials have demonstrated that therapeutic hypothermia can be effective3 if it is initiated within 6 hours after birth and lasts for about 72 hours.
- Stem Cell Therapy for HIE has been given together with hypothermia in more than a half dozen clinical trials worldwide4. The stem cells are harvested from the baby’s own umbilical cord blood and given back to the baby intravenously. Duke University has published5 results from their first trial and they are currently recruiting patients for a phase 2 trial.
References
- Patel Y & Rumore MM. Pharmacy and Therapeutics 2012; 37(7):405–411.
- AMAG press release 14 Feb 2018
- Bonifacio SL et al. Nature Reviews Neurology 2011; 7:485–494.
- Data accessed from CellTrials.org
- Cotten CM et al. Journal of Pediatrics 2014; 164(5):973–979.



 The
The