You are here
Cord Blood Collection Kits
Many parents elect to save their newborn infant's umbilical cord blood in either a public cord blood bank that accepts free donations or a family cord blood bank that charges for private storage. Typically the first step towards banking cord blood is when the mother receives a collection kit that she must safeguard and have ready at the time of birth. This article explains the contents of collection kits and gives parents advice on how to keep them safe.
 Cord blood collection kits make cord blood storage options available to many expectant mothers. Most public cord blood banks only accept donations from a limited number of large hospitals where they have staff to collect the cord blood. By comparison, the collection kit model of cord blood banking can be used in a wider variety of settings and locations. The mother's healthcare provider performs the collection, and hence should be trained in the optimum collection procedures. The kit contains the supplies that are needed at the time of birth, and it is designed to protect the cord blood during transport to the laboratory. Family cord blood banks all rely on collection kits. A few public cord blood banks offer parents the option to donate their baby's cord blood, at no cost to the family, with a mail-in collection kit.
Cord blood collection kits make cord blood storage options available to many expectant mothers. Most public cord blood banks only accept donations from a limited number of large hospitals where they have staff to collect the cord blood. By comparison, the collection kit model of cord blood banking can be used in a wider variety of settings and locations. The mother's healthcare provider performs the collection, and hence should be trained in the optimum collection procedures. The kit contains the supplies that are needed at the time of birth, and it is designed to protect the cord blood during transport to the laboratory. Family cord blood banks all rely on collection kits. A few public cord blood banks offer parents the option to donate their baby's cord blood, at no cost to the family, with a mail-in collection kit.
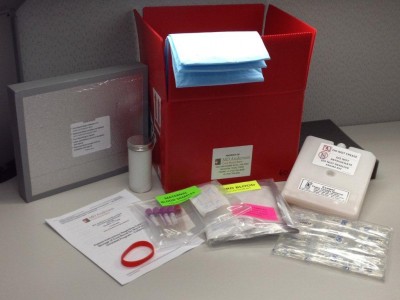
Since public cord blood banks have more stringent requirements than family banks, this article will focus on their mail-in collection kits. In order to mail in a cord blood donation, the expectant mother must meet the donation guidelines, pass a health history screening, and her obstetrician or midwife must complete the required training and accept responsibility to collect the cord blood. Once approved for mail-in donation, the mother receives a collection kit about two weeks before the baby's expected birth date. The collection kit consists of a shipping box containing the following:
- all supplies required to collect the umbilical cord blood from the baby,
- all supplies required to collect blood samples from the mother,
- collection instructions,
- temperature logger,
- return shipping materials,
- return address labels to ship the kit to the blood bank,
- instructions to the mother for storage of the kit before the birth of her baby, and
- instructions on how to pack the cord blood and maternal blood and ship the kit.
 Proper storage of the collection kit before the birth of the baby is just as important as shipping and handling of the kit afterward. Parents should pay attention to and follow the instructions that come with the kit. The blood vials and blood bag inside the kit contain anti-coagulants that prevent blood from clotting while the kit is being shipped to the lab. To preserve the performance of these chemicals, the kit must not be frozen, refrigerated, kept in direct sunlight, stored in the trunk of a car, or any other scenario that will subject the contents to extreme temperatures. Nor should parents open the kit and remove any supplies. The shipping box is designed to protect the supplies and maintain an even temperature. The best way for the mother to safeguard the collection kit is to keep it indoors, so that the kit stays within the same range of temperatures that a person would find comfortable. She can keep the kit with her, or she can rely on a close friend or family member to bring it to the hospital as soon as the goes into labor.
Proper storage of the collection kit before the birth of the baby is just as important as shipping and handling of the kit afterward. Parents should pay attention to and follow the instructions that come with the kit. The blood vials and blood bag inside the kit contain anti-coagulants that prevent blood from clotting while the kit is being shipped to the lab. To preserve the performance of these chemicals, the kit must not be frozen, refrigerated, kept in direct sunlight, stored in the trunk of a car, or any other scenario that will subject the contents to extreme temperatures. Nor should parents open the kit and remove any supplies. The shipping box is designed to protect the supplies and maintain an even temperature. The best way for the mother to safeguard the collection kit is to keep it indoors, so that the kit stays within the same range of temperatures that a person would find comfortable. She can keep the kit with her, or she can rely on a close friend or family member to bring it to the hospital as soon as the goes into labor.
The collection kit contains a temperature logger that monitors the temperature inside the box from the time it leaves the cord blood bank until it is returned to the bank. This is another reason why supplies should not be removed from the kit. The temperature logger is set by the bank, so it does not need to be turned on or off by the mother or the hospital staff. When the mother goes to the hospital to give birth, only then is the kit handed over to the hospital staff.
 Cord blood is collected immediately after the birth of the baby. At that time, the healthcare provider who has trained to perform the collection will use the supplies in the kit to collect as much umbilical cord blood as is feasible. Blood samples are also collected from the mother at the time of birth. The healthcare provider completes the forms in the kit and labels the cord blood collection bag with the mother's identification details, which normally is the mother's hospital label. The labeled collection bag is placed into a zip-seal bag. If the collection bag is not labeled, the donated blood will be discarded upon receipt at the cord blood bank.
Cord blood is collected immediately after the birth of the baby. At that time, the healthcare provider who has trained to perform the collection will use the supplies in the kit to collect as much umbilical cord blood as is feasible. Blood samples are also collected from the mother at the time of birth. The healthcare provider completes the forms in the kit and labels the cord blood collection bag with the mother's identification details, which normally is the mother's hospital label. The labeled collection bag is placed into a zip-seal bag. If the collection bag is not labeled, the donated blood will be discarded upon receipt at the cord blood bank.
Finally, the cord blood must be shipped to the lab. The bag holding the baby's cord blood and the vials holding the mother's blood samples are packaged back into the shipping box according to the instructions. Again it is important to keep the contents of the box close to room temperature. The packaging is designed to maintain an even temperature during transport and to protect the blood samples during routine handling. The cord blood must be shipped to the bank as soon as possible, so that it arrives within the specified time (normally 36 hours from the time of collection). If the donation arrives after the specified time, the stem cells in the cord blood may no longer be viable and cannot be stored.
 When parents choose to donate their baby's cord blood, they give birth to hope for others at the same time that they welcome a new life into their family. Parents can arrange for a friend or family member to take responsibility for packing and shipping the collection kit, so that they can focus on their new baby. The hospital staff generally does not have time to perform this task. Collection kit instructions are simple and the kit is robust if it is not abused. Proper handling of the collection kit insures that the irreplaceable cord blood reaches the bank in the best possible condition to provide healthy cells that have the ability to do what they need to do when the time comes.
When parents choose to donate their baby's cord blood, they give birth to hope for others at the same time that they welcome a new life into their family. Parents can arrange for a friend or family member to take responsibility for packing and shipping the collection kit, so that they can focus on their new baby. The hospital staff generally does not have time to perform this task. Collection kit instructions are simple and the kit is robust if it is not abused. Proper handling of the collection kit insures that the irreplaceable cord blood reaches the bank in the best possible condition to provide healthy cells that have the ability to do what they need to do when the time comes.