You are here
Accessing the Value of Cord Blood Therapies
 |  |  |  |
There is growing acceptance in the medical community that stem cells derived from cord blood have value as a therapy for pediatric neurologic injury. But what financial hurdles do parents face when they attempt to access that value for their children? In this article we present a case study of the out-of-pocket costs that parents face when they use their child's own (autologous) cord blood as therapy for cerebral palsy, and receive the treatment at Duke University Medical Center ("Duke" hereafter).
Dr. Kurtzberg's group at Duke pioneered the use of cord blood transplants to cure children suffering from metabolic disorders such as leukodystrophies and storage diseases. Along the way, the researchers found that children receiving cord blood transplants also experienced significant improvements in their motor and cognitive skills, and these improvements were more marked in children who were younger when they received the transplant (Escolar et al. 2005). In two cases where a transplanted child later died, autopsies revealed that cells grown from the donor lineage had taken up residence in the patient's brain.
The surprising neurologic improvements seen in children receiving cord blood transplants led to the proposal to give cord blood stem cells to children with brain injuries. At this time, the evidence that stem cells in cord blood can repair brain injury is as follows:
- Cord blood contains anti-inflammatory cells that could inhibit the inflammatory response after acute injury
- Cord blood may contain cells that induce endogenous repair via a cellular or paracrine effect
- Cord blood contains neural cell progenitors that could facilitate repair and regeneration
- Cord blood cells cross the blood brain barrier (Kurtzberg et al. 2003; Abstract222 BBMT 9.2:128)
- Cord blood cells reach the brain and improve motor function in rabbit pups with brain injury (Tan et al.)
Cerebral palsy is a diagnosis that covers a variety of sequelae to brain injury that occurred at a very young age: in utero, at birth, or in infancy. The actual cause of the injury could be bleeding in the brain (stroke), excessive pressure from fluid in the brain (e.g. hydrocephalus), loss of oxygen, traumatic brain injury, etc. The clinical symptoms of cerebral palsy may include impaired movement associated with exaggerated reflexes, floppiness or rigidity of the limbs and trunk, abnormal posture, involuntary movements, unsteadiness of walking, or some combination of these. Children with cerebral palsy often have learning disabilities as well. We discuss the incidence of cerebral palsy more in the next article, but will note here that in the United Sates about 1 in 300 children have cerebral palsy (CDC).
Starting in 2004, Dr. Kurtzberg's group at Duke began giving cord blood therapy to children who had brain injuries. In order to demonstrate safety, the children were treated with their own (autologous) stem cells, so there could not be any adverse reactions to donor (allogeneic) stem cells. This meant that the only children eligible for treatment were those whose parents had privately stored their cord blood at birth in a family cord blood bank. Nonetheless, word of the program spread and children with these diagnoses have traveled from all corners of the world to receive treatment at Duke. A pipeline of children also entered the program through partnerships with public cord blood banks who held cord blood in reserve for babies that were born at risk.
In 2010 this clinical program reached two milestones: One was the publication of a paper in the journal Transfusion that covered the first 184 patients treated at Duke for various acquired neurologic disorders (Sun et al. 2010). This paper reviewed the quality of the family cord blood units that were sent to Duke. Fundamentally, the ability of children to access therapy with their own cord blood rests on the quality of their stored cord blood. It is vital that family cord blood banks maintain high standards so that their clients have enough viable stem cells for future therapy.
The second milestone in 2010 was the launch of a Phase 2 clinical trial for spastic cerebral palsy, a category which comprises about 80% of children with cerebral palsy (CDC). Having already demonstrated that cord blood therapy for cerebral palsy was safe, this trial was designed to measure the efficacy of the treatment against a control. All children in the trial receive the benefits of cord blood therapy, but they are divided into two arms that cross over after one year: the study group receives stem cells in their first infusion and a placebo after one year, whereas the control group receives the placebo first and the stem cells one year later. Moreover, the trial is double blind so that neither the families nor their care givers should know which group is which. The trial was designed to enroll 120 children, and by the end of 2013 had achieved 65% accrual, with 40 patients who had completed their one year follow-up visit. Between this and other clinical trials, plus children who do not meet any trial enrollment criteria but receive compassionate care off-trial, Dr. Kurtzberg estimates that about 125 children per year receive autologous cord blood therapy at Duke.
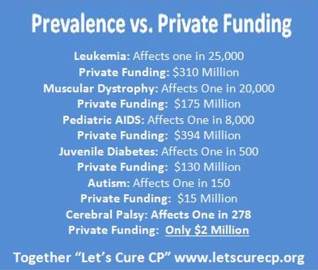
Raising funding for research on stem cell therapy for pediatric brain injury is an ongoing challenge. While cerebral palsy affects more individuals in the US than childhood diabetes and childhood leukemia combined, it does not receive the same research dollars as those high profile diseases. The accompanying infographic from the charity Let's Cure CP charts prevalence versus private funding for several pediatric disorders, demonstrating that cerebral palsy research is relatively under-funded. The program at Duke was very fortunate to receive a generous grant from the Julian Robertson Foundation, but they constantly need more funding to conduct more pre-clinical studies and launch new trials.
The charity Let's Cure CP was launched by parents who refused to accept the status quo. For years, fact sheets about cerebral palsy have said that "At this time, there is no cure for the developmental brain damage that causes cerebral palsy". But, with advances in stem cell therapy, perhaps cerebral palsy can indeed be cured or at least significantly ameliorated.
The mission of Let's Cure CP is to raise funding for clinical trials of stem cell therapy for cerebral palsy. The net hospital cost for each patient in these trials is about $35,000 (reference: Let's Cure CP), but much of that price is due to the high cost of brain imaging studies. At Duke, the patient testing, medical care, and cord blood infusion alone cost about $7,000. The main question burning in the mind of patient advocates is: How much of this cost gets passed on to patient families? Answering that question is the heart of this article.
We have compiled a table showing the real costs incurred by real patients who traveled to Duke to receive autologous cord blood therapy for cerebral palsy. The US and Mexico data come from families that cooperated with Let's Cure CP, and the overseas data come from cord blood banks that cooperated with Parent's Guide to Cord Blood Foundation. All costs have been converted to US dollars at the current exchange rates. The net treatment-related costs vary from zero to about $13,000, plus each family also paid travel costs. The four key variables in the costs are: 1. whether the patient's treatment was on- or off-trial, 2. whether the cord blood bank covered the cost of shipping the cord blood, 3. the patient's type of medical insurance coverage, and 4. the travel distance. We explain these in turn.
Real Costs to Real Patients (USD):
autologous cord blood therapy for cerebral palsy at Duke
| On-Trial? | Nationality | Cost of Family Travel | Cost of Cord Blood Shipping (* = paid by bank) | Cost of Medical Care at Duke |
| YES | USA | $1,000 | $3,000 | $0 |
| YES | Italy | $3,300 | $2,275 * | $0 |
| YES | Romania | $8,400 | $2,422 * | $0 |
| YES | New Zealand | over $7,800 | $3,000 * | $0 |
| NO | USA | $1,200 | $3,000 | $25 |
| NO | USA | $1,300 | $unknown | $7,000 |
| NO | USA | $2,000 | $unknown | $7,300 |
| NO | Mexico | $3,000 | $2,000 | $1,400 |
| NO | Romania | $8,400 | $2,800 * | $9,450 |
| NO | New Zealand | over $7,800 | $3,000 * | $11,000 |
Trial Participation: Patients who meet the eligibility criteria to participate in the clinical trial for spastic cerebral palsy have all of their medical costs covered by the trial funding, regardless of their nationality. In addition, all families on-trial receive a flat travel stipend to defray the cost of bringing their child to Duke for evaluation and treatment. Patients coming from outside the US are asked to pay an up-front deposit that covers their estimated hospital costs, but if they are on-trial they are later reimbursed.
Cord Blood Shipping: When cord blood is released from a bank for therapy, it is shipped frozen to the treatment hospital in a small cryotank called a "dry shipper" and is only thawed before therapy. The cost to have a medical courier transport cord blood to Duke in a dry shipper should only be a few hundred dollars to cross the US, but runs into thousands of dollars to cross oceans on connecting flights. Moreover, since the dry shipper is the property of the bank, it must make a return trip too - but this costs much less because it is no longer carrying a medical shipment.
The cost impact of shipping cord blood varies greatly among patient families. Previously, when it was rare for family banks to release cord blood for therapy, they routinely covered this cost as part of their profit margin. Now that the bigger family banks are releasing multiple therapies per year, some companies have stopped covering this cost. Parents should ask questions about bank policy on the cost of shipping released cord blood before signing a contract for private storage with a family bank.
Cost of Medical Care at Duke: The policy at Duke Medical Center is to "accept assignment" for these patients, which is insurance industry terminology for accepting whatever payment the patient's medical insurance policy is able to pay. But patients coming to Duke from outside the US usually do not have any insurance coverage for treatment at Duke. These patients must pay deposits to cover the estimated full cost of the infusion process, which for the families we talked to ranged between $7,000 and $13,000. One family we spoke to had dual residence in Mexico and the US and was able to obtain insurance coverage for therapy. Even for families who are based within the US, there is a large variation in patient out-of-pocket costs, because in this country there is a large varation in the deductibles of medical insurance policies.
Duke does have a charity program that will cover healthcare costs for eligible families who are paying for therapy out-of-pocket and cannot afford their child's care. In order to qualify for the charity program, the family must go through an application process and fully disclose their financial status. But, even in the charity program, US law inhibits hospitals from waiving insurance deductibles due to risk of legal exposure.
Cost of Family Travel: Obviously, the young children in this study could not travel unaccompanied. Every family paid travel costs for the patient and at least one other family member. The in-trial patients received a travel stipend of $1,000 per visit. Families receiving treatment at Duke can find affordable housing at the local Ronald McDonald House, or at one of the local hotels where Duke has arranged discount prices that cover the room and breakfast. Nonetheless, travel was a significant expense for all families, especially those coming from overseas.
The final topic in our discussion is the need for a new type of health insurance policy that will cover patients who require stem cell therapy and who may need to travel across borders to receive such treatment. Patients may have a national health plan, an employer-provided insurance policy, or a privately purchased insurance policy, but there may be gaps in their coverage for specialized medical care, which may include a need to procure alternative units of cord blood, a need for repeat transplants, and perhaps costs associated with surgery in an alternate location. To address these situations, some cord blood banks have partnerships with insurance providers that offer their clients coverage for therapy using the child's cord blood.
In conclusion, we have compiled real patient costs for cerebral palsy therapy at the leading treatment center and found that, while it is much less expensive than rumored, the out-of-pocket costs vary widely between families due to differences in patient insurance coverage. The health insurance industry needs to evolve away from a silo model where coverage is restricted to the patient's home nation, and offer insurance products more in tune with the international nature of medical research, where patients cross international borders either to access clinical trials or to access standard therapies at centers of excellence.


