You are here
Placenta Position and When it Matters
Expectant parents may hear a lot of rumors saying that the position of the placenta inside the uterus is important for the progress of the pregnancy or the ability to have a vaginal birth. Fortunately, most of the “old wives’ tales” about placenta position are not supported by a review of articles in peer-reviewed medical journals. Here we discuss a few of these topics.
Names of Placenta Positions
Wherever the fertilized egg happens to land in the uterus, it will become anchored to that spot and form a placenta. The placenta starts as a few cells that separate from the fertilized egg and burrow into the uterine lining1-3. Between weeks four and twelve of gestation, the placenta becomes fully developed, and at the beginning of the second trimester the placenta takes over producing the hormones needed to sustain the pregnancy3-5. The placenta development phase between weeks four and twelve is suspected to be a big source of first trimester pregnancy fatigue4,5. Throughout the rest of the pregnancy the placenta will gradually grow with the baby.
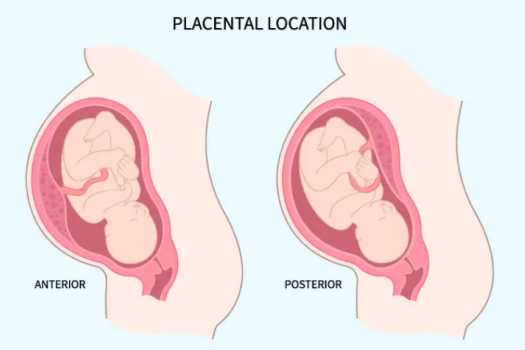
The names that your doctor might note in your chart to describe the position of the placenta are as follows:
- Anterior Placenta – The placenta is on the front wall of the uterus, by the outside of the mother’s body.
- Posterior placenta – The placenta is on the back wall of the uterus, towards the mother’s spine.
- Lateral Placenta – The placenta is on the side of the uterus, either left or right.
- Fundal Placenta – The placenta is at the top of the uterus. The word “fundus” is a medical term for the part of an organ that is opposite the opening.
- Low-Lying Placenta – The placenta is below the mid-line of the uterus. Doctors do not agree on a universal definition of how low is “low-lying”.
- Placenta Previa – The placenta is partially or fully covering the cervix, the opening through which the baby is born in a vaginal delivery.
How do you know where your placenta Is located?
In the US, expectant mothers that are under the care of an obstetrician will usually have two ultrasounds during pregnancy6. The location of the placenta can be accurately determined as early as 10 weeks gestation. In fact, during the first trimester the placenta is bigger than the baby7.
It is difficult for a midwife or the mother herself to tell where the placenta is located just by feel. Late in pregnancy, a midwife can certainly tell you how the baby is positioned. It is hard to feel the placenta because it is not a distinct bump, it is a thickening of the uterine wall, and by the end of pregnancy it is about an inch thick and 10 inches across1.
When the placenta is in front, called anterior placenta, the extra cushioning means that the baby’s kicks do not feel as strong against the mother’s abdomen. Some mothers think they can tell the difference, but you always have to wonder if this baby is kicking less hard because the placenta is anterior, or is this baby kicking less hard because it is a different baby?
What placenta position is most common?
There is a lot of confusion about which placenta position is the most common. The reason for this is a lack of consensus in the medical literature. There are published research studies that conclude anterior is the most common, but other studies find posterior is the most common8,9. Also, many medical studies do not even distinguish between anterior versus posterior placenta, they only distinguish between placenta locations that are safe for vaginal delivery versus unsafe. It is fair to say that both anterior and posterior placenta each represent about 40-45% of pregnancies, with the other positions being uncommon.
The lateral placenta position only occurred 3.6% of the time in a 2025 statistical review of 40 previous studies covering over 98 thousand pregnancies10. The vast majority of placentas in the review were either anterior or posterior. This review also did not see any significant relationship between placenta position and the ability of the baby to flip head down in time for birth (which doctors call cephalic presentation)10.
Placenta Migration
The placenta is said to migrate upwards over the course of pregnancy. The word “migration” is a bit of a misnomer, because the placenta is anchored to the uterine wall and does not move, but the walls of the uterus stretch during pregnancy, causing the relative position of the placenta to move up. This is very helpful, because having a placenta which is low-lying, near the cervix, is a risk factor for bleeding during birth.
In 2019, a meta-analysis of 11 previous studies holding 3586 pregnant women confirmed that when a low-lying placenta is detected in the second trimester, over 63% of the time it had migrated out of the risk zone by the third trimester11. Some studies found that an anterior placenta tends to migrate more than a posterior placenta, but once again the studies did not uniformly agree on this11-13.
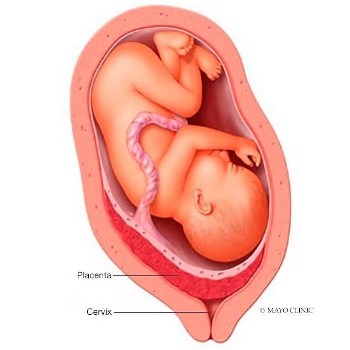 Placenta Previa
Placenta Previa
The name placenta previa applies to any situation where the placenta overlaps the cervix; the three degrees of placenta previa are marginal, partial, and full. This situation is rare; one retrospective study of over 93 thousand deliveries at a single maternity hospital found that placenta previa only occurred in 0.55% (about 1 in 200) of pregnancies14.
Placenta previa is a serious concern. The most recent meta-analysis of previous studies found that the risk of postpartum hemorrhage (medical term is PPH) is 49% higher when the placenta is low-lying10,15. With placenta previa, there is a risk that during labor part of the placenta will separate prematurely from the uterine wall, which is called placental abruption. A warning sign of placental abruption is bleeding during pregnancy. A full separation is a full-fledged emergency, because it cuts off the baby’s oxygen supply. Given all the risks, “nearly all women with placenta previa” will need to deliver the baby by C-section16.
Placenta Position Post C-Section
For the past 15 years, the percentage of babies in the US that are born by C-section has been holding steady at about 32%17,18. This means that about one third of mothers that are pregnant with a second child had a C-section the first time. Obstetricians typically make the C-section incision along the “bikini line”, a low transverse cut that is parallel to the abdominal muscles, and is also low-lying on the uterus19. Once a mother has had a C-section, there is an area of scar tissue on her uterus, and future pregnancies will not implant and form a placenta in that location. The bikini line incision leaves the entire upper body (corpus) of the uterus available for future placenta implantation.
Mothers that have had a C-section have an elevated risk of placenta previa, where the fertilized egg implants below the C-section scar and the placenta overlaps the cervix19-21. A landmark paper published in 1997 by researchers at the Robert Wood Johnson Medical School reviewed 36 studies covering a total of 3.7 million pregnant women, out of which 13,992 patients were diagnosed with placenta previa20. They found that the overall incidence of placenta previa was approximately 1 in 200 deliveries, but women with a prior C-section had a higher risk for placenta previa in a subsequent pregnancy20. A follow up paper published by the same research group in 2006 used more advanced statistics to refine their calculation of risk. They found that after a single C-section the risk of placenta previa increased by a factor of 1.6321. This study also demonstrated that the risk of placenta previa goes up with each C-section. For example, if the first two births were by C-section, then the risk for placenta previa doubled in the third pregnancy, from 1 in 200 to 2 in 20021.
The risk of placenta previa is still small for mothers that have had C-sections, and of course your obstetrician is aware of these possible complications and will keep an eye on your pregnancy. Public health officials argue that the rate of C-section deliveries should be reduced to avoid the difficulties that can occur in subsequent births.
References
- Cleveland Clinic. Placenta. Health Library. Last reviewed 2022-02-04
- de Bellefonds C, Wu J. What Is the Placenta? What This Organ Does and How It Forms. What to Expect. Published 2021-07-09
- Boss AL, Chamley LW, James JL. Placental formation in early pregnancy: how is the centre of the placenta made? Human Reproduction Update. 2018; 24(6):750–760.
- de Bellefonds C, Payson M. Fatigue During Pregnancy. What to Expect. Published 2022-11-17
- Bai G, Korfage IJ, Hafkamp-de Groen E, Jaddoe VWV, Mautner E, Raat H. Associations between Nausea, Vomiting, Fatigue and Health-Related Quality of Life of Women in Early Pregnancy: The Generation R Study. PLOS 2016; 11(11): e0166133.
- UPMC Magee-Womens Hospital in Pittsburgh. What Is the Typical Pregnancy Ultrasound Schedule? Health Beat. Published 2023-05-08
- Fadl S, Moshiri M, Fligner CL, Katz DS, Dighe M. Placental Imaging: Normal Appearance with Review of Pathologic Findings. 2017; RadioGraphics 37(3):
- Alikhani F, Aalinezhad M, Bahrami M, Geravandi M. Placenta location, a prognostic determinant for the incidence of preeclampsia. BMC Pregnancy Childbirth 2024; 24:835.
- Jansen CHJR, Kleinrouweler CE, Kastelein AW, Ruiter L, van Leeuwen E, Mol BW, Pajkrt E. Follow-up ultrasound in second-trimester low-positioned anterior and posterior placentae: prospective cohort study. Ultrasound in Obstet. & Gyn. 2020; 56:725-731.
- Whitcombe DD, Hu Z, Ounpraseuth ST, Magann EF. Placental Location Site and Associated Intrapartum, Postpartum, and Neonatal Complications: A Comprehensive Review and Meta-Analysis. Journal of Clinical Medicine. 2025; 14(5):1649.
- Jansen CHJR, Kleinrouweler CE, van Leeuwen L, Ruiter L, Limpens J, van Wely M, Mol BW, Pajkrt E. Final outcome of a second trimester low-positioned placenta: A systematic review and meta-analysis. European J. Obstetrics & Gyn. Reproductive Bio. 2019; 240:197-204.
- Cho JY, Lee YH, Moon MH, Lee JH. Difference in migration of placenta according to the location and type of placenta previa. J Clinical Ultrasound. 2008; 36(2):79-84.
- Pradhan S, Tuladhar A, Shrestha A, Amatya NB, Pradhan P. Sonographic assessment of placental migration in second trimester low lying placenta. Nepal Med. College J. 2012; 14(4):331-333.
- Frederiksen MC, Glassenberg R, Stika CS. Placenta previa: A 22-year analysis. Amer. J. Obstetrics Gynecology. 1999; 180(6):1432-1437.
- Fan D, Xia Q, Liu L, Wu S, Tian G, Wang W, Wu S, Guo X, Liu Z. The Incidence of Postpartum Hemorrhage in Pregnant Women with Placenta Previa: A Systematic Review and Meta-Analysis. PLOS. 2017; 12(1):e0170194.
- Mount Sinai. Placenta previa. Health Library. Accessed 2025-04-01.
- Solheim KN, Esakoff TF, Little SE, Cheng YW, Sparks TN, Caughey AB. The effect of cesarean delivery rates on the future incidence of placenta previa, placenta accreta, and maternal mortality. J Maternal-Fetal & Neonatal Med. 2011; 24(11):1341-1346
- Centers for Disease Control and Prevention (CDC). Births – Method of Delivery. FastStats. Last Updated 2024-04-09
- Mayo Clinic. C-section. Tests & Procedures. Published 2022-06-16
- Ananth CV, Smulian JC, Vintzileos AM. The association of placenta previa with history of cesarean delivery and abortion: A metaanalysis. 1997; AJOG 177(5):1071-1078.
- Getahun D, Oyelese Y, Salihu HM, Ananth CV. Previous cesarean delivery and risks of placenta previa and placental abruption. Obstet. Gynecol. 2006; 107(4):771-778.


