You are here
Myth: Cord Blood has Less Engraftment than Haplo Transplants
Today we look at a myth that persists in the medical community and that hampers the willingness of oncologists to transplant cord blood. That myth is the belief that cord blood is slower to engraft and has a higher graft failure rate than other graft sources.
It is important to start by defining the term engraftment. When a patient goes through a stem cell transplant, they first receive intense chemotherapy to wipe out their immune system. Then they receive a graft of stem cells from a donor. As the newly infused cells start to grow, they first repopulate the bone marrow, and then reconstitute the patient’s immune system. The first cell group to grow back is a type of white blood cells called neutrophils. The metric for “engraftment” is to have an Absolute Neutrophil Count (ANC) over 5001.
There are two parameters of engraftment that are important. One is whether the graft fails to take hold at all, which is called graft failure. The other is how long it takes to reach ANC > 500, which is called engraftment time.
In the early years of cord blood transplants, it was found that the cord blood infusion failed to engraft about 11% of the time2. This made cord blood a higher risk transplant option. Whereas you can go back to an adult donor and ask for more stem cells to try again, you cannot go back to the same cord blood donor to get more. The fallback option would be to get another cord blood unit from a different donor. As a result, the mindset developed among transplant doctors to use adult donors wherever possible and only resort to cord blood when a matching adult donor was not available.
Nonetheless, cord blood was the best transplant option for patients that lacked a fully matched adult donor for about a quarter of a century. This was because partially matched cord blood could be given to patients with rare genetic types without risk of severe graft versus host disease. This provided a transplant option for patients from rare and mixed racial backgrounds who could not find an exactly matched adult donor. Then, in the mid 2010’s, a new protocol for preventing graft versus host disease after stem cell transplants was invented3. The new approach was to give patients Post-transplantation Cyclophosphamide, abbreviated as PCy. The concept of giving a chemotherapy drug after the graft had been delivered seemed radical at the time. But PCy acts to suppress T-cells that react against genetic differences between the donor and the patient. Thanks to PCy, it became possible to give patients stem cells from half-matched adult donors, which many people can find among their siblings and parents3. These are called haploidentical or “haplo” transplants. Since then, haplo transplants have become the dominant treatment for patients that lack fully matched donors, and the use of cord blood transplants has declined4.
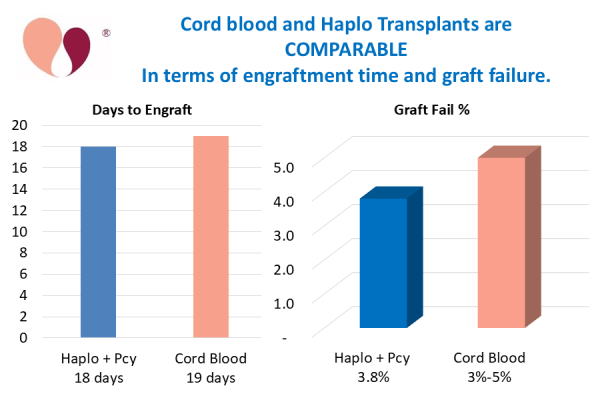
An expert review of three decades of cord blood transplants has provided statistics on how cord blood graft failure has decreased with time5. In the most recent time interval, engraftment was examined for 1802 patients receiving a single unit cord blood transplant. Provided that the patient received a cell dose over 25 million TNC/kg, then the engraftment rate was 95%5. The engraftment rate went up to 97% if the transplant also had a 6 out of 6 HLA match between patient and donor5. Put the other way, the graft failure rate was only 3% to 5%. This is comparable to the 3.8% graft failure rate of haplo transplants that was determined in a retrospective study of 958 patients at an expert treatment center6.
Another important comparison between cord blood transplants and haplo transplants is the time to engraftment. For cord blood transplants, the median time to neutrophil engraftment has improved substantially, falling from 25 days during the early transplants down to 19 days currently5. Transplants of adult sources of stem cells, such as bone marrow and peripheral blood, are known to have a median engraftment time of 16 days7. But, when PCy is given after a transplant to suppress graft rejection, it slows down the engraftment of haplo transplants, depending on the timing and doses of PCy and other drugs given as prophylaxis against graft versus host disease8. A recent review of haplo transplants given to 509 patients to treat acute leukemia in Europe found engraftment times of 18-19 days8. Thus, cord blood and haplo transplants are now comparable in engraftment speed.
In conclusion, transplant doctors should not just assume that cord blood is the second-best choice of graft source for their patients. A known advantage of cord blood transplants is that they have lower incidence of chronic graft versus host disease than haplo transplants, which could provide patients with better long-term quality of life5,8. Hopefully transplant providers can be encouraged to widen the scope of factors that are considered in their treatment decisions.
References
- Raymaakers K. Engraftment in a Stem Cell Transplant. Verywell Health A-Z Updated 2023-01-20
- Wagner JE Jr., Eapen M, Carter S, Wang Y, Schultz KR, Wall DA, .... Kurtzberg J. One-Unit versus Two-Unit Cord-Blood Transplantation for Hematologic Cancers. NEJM. 2014; 371:1685-1694.
- Fuchs EJ. Related haploidentical donors are a better choice than matched unrelated donors: Point. Blood Advances 2017; 1(6):397-400.
- World Marrow Donor Association. WMDA Global Trends Report. Published 2024-05-30
- Kurtzberg J, Troy JD, Page KM, El Ayoubi HR, Volt F, Scigliuolo GM, … Gluckman E. Unrelated Donor Cord Blood Transplantation in Children: Lessons Learned Over 3 Decades. Stem Cells Translational Medicine. 2023; 12(1):26–38.
- Mata JR, Zahurak M, Rosen N, DeZern AE, Jones RJ, Ambinder AJ. Graft Failure Incidence, Risk Factors, and Outcomes in Patients Undergoing Non-Myeloablative Allogeneic Hematopoietic Cell Transplantation Using Post-Transplant Cyclophosphamide. Transplantation and Cellular Therapy 2024; 30(6)588-596.
- Eapen M, Rubinstein P, Zhang M-J, et al. Outcomes of transplantation of unrelated donor umbilical cord blood and bone marrow in children with acute leukaemia: a comparison study. Lancet 2007; 369(9577):1947-1954.
- Ruggeri A, Labopin M, Battipaglia G, Chiusolo P, Tischer J, Diez-Martin JL, ... Mohty M. Timing of Post-Transplantation Cyclophosphamide Administration in Haploidentical Transplantation: A Comparative Study on Behalf of the Acute Leukemia Working Party of the European Society for Blood and Marrow Transplantation. Biol. Blood Marrow Transpl. 2020; 26(10):1915-1922.


