You are here
Cryopreserved Amniotic Membrane in the Treatment of Keratitis
Advisory: At the end of this article is a series of case reports that display photos of eyes healing after successful surgery with amniotic membrane transplants.
Keratitis is an inflammation of the cornea that can have several causes, including bacterial infection, viral infection, and eye injury. Severe cases of keratitis result in a corneal ulcer. This article reports on a clinical study in Ukraine that treated keratitis patients with cryo-preserved amniotic membrane.
The Ukraine study was a collaboration between clinicians that are expert in treating eye disorders and a biobank that provided the amniotic membrane. Team members from the Filatov Institute of Eye Diseases and Tissue Transplantation of the Academy of Medical Sciences (AMS) in Odessa: Drozhzhyna G. I., Sereda K. V., and Gaidamaka, T. B. Team members from Ukraine’s first biobank at the Institute of Cell Therapy: Nemtinov P.I., Shablii V.A., Nasadyuk C.M., Makhinya A.V., and Martynenko S.I.
The shortage of cornea donations for use in eye surgery has led to a great interest in applications of amniotic membrane for ophthalmology. Preclinical studies of cryopreserved amniotic membrane in rabbits with experimental bacterial keratitis have demonstrated its elasticity and its ability to promote wound healing. Some clinical trials in humans have also demonstrated a prominent anti-inflammatory effect of the donated amniotic membrane and rapid re-epithelization in treatment of ulcerative keratitis.
During 2016-2018 the team in Ukraine conducted a phase 1/2 study titled “Application of the Human Cryoconserved Amniotic Membrane in Keratitis of Infectious and Neurotrophic Ethiology”. The study included 27 consenting patients of both genders, aged 20-40, with diagnoses of bacterial, neurotrophic, and herpetic keratitis. The study excluded pregnant or lactating women, patients with severe complications of the keratitis (corneal perforation with diameter more than 2.0 mm), corneal abscess, endophthalmitis, uncompensated glaucoma, retinal detachment, and the presence of other diseases that could have significant effect on the results of treatment (stroke, uncompensated diabetes, myocardial infarction, malignant disease, HIV or syphilis).
The study of amniotic membrane application in the surgical treatment of keratitis was divided into three experimental groups. In each group, treatment was performed without HLA-typing of the amniotic membrane or immune-suppression of the patient. Each of the three groups received a different type of amniotic membrane transplant (AM transplant).
Study Group 1 received “inlay” AM transplant. The amniotic membrane was inlaid into the zone of damaged cornea, without coverage of the intact zone. Amniotic membrane was fixed with separate stitches and played the role of basal membrane, stimulating the epithelium cells to grow in the defect zone.
Study Group 2 received “onlay” AM transplant. The entire corneal surface was covered by the amniotic membrane (biological coverage), which was fixed in place with episcleral interrupted stitches. In this case, the amniotic membrane played a role in healing the entire cornea, not just the defect zone.
Study Group 3 received a ”sandwich” AM transplant. In the combined sandwich technique, both the inlay and onlay methods were used. The amniotic membrane was first inlaid and fixed to the corneal tissue defect, and a second layer of amniotic membrane covered the entire cornea with the help of episcleral fixation.
No complications or side effects were noted either during or after surgery with the cryopreserved human amniotic membrane. The outcomes of the AM transplants were evaluated at 1, 3, 6, 12, 18 and 24 months after the procedure and the following criteria were determined:
- Hospitalization
- Implant detachment and resorption
- Local, regional and systemic infections, associated with implant
- Induced neovascularization of the cornea
- Tumor formation
- Changes in pain syndrome
- Epithelization of the corneal surface
- Changes in vison
- Changes in corneal transparency
- Changes in “dry eye syndrome” manifestation
- Resorption of corneal stroma infiltration
The results of the clinical trial showed that transplantation of the amniotic membrane is a safe and effective method of treating corneal inflammation. The AM transplant enhances rapid improvement of the inflammatory process, with the average resorption of corneal infiltration on day 4.3 (SD = 5.07) and the average regression of stromal edema on day 9.3 (SD = 3.6). At the time of hospital discharge, 25 of 27 patients (92.6%) exhibited a positive therapeutic effect. By one month after surgery, the intensiveness of corneal vascularization had decreased by 11.2% within 1-2 quadrants, and was down by 22.3% within 3 and more quadrants. It is important that the amniotic membrane encourages epithelial (skin) cells to grow on the surface of the cornea without the development of vascularization (blood vessel growth). After 3 months, the re-epithelization of the cornea had been achieved in 26 patients (96.3%) that had originally presented with keratitis.
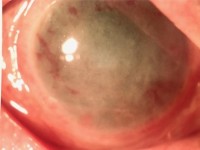
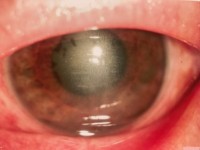
Clinical Case 1: Patient S., 63 years old. Two-sided neurotrophic keratitis. Transplantation of the amniotic membrane was performed on both eyes.
Photo ОD. Erosion of cornea, infiltration and edema of the stroma. Vision = 0.005 | Photo ОS. Subtotal corneal erosion, edema of the stroma. Vision = 0.02 | |
Photo ОD. 1 day after AM transplant | Photo ОS. 1 day after AM transplant | |
Photo OD. 1 month after AM transplant | Photo ОS. 1 month after AM transplant | |
Photo OD. 3 months after AM transplant. Vision = 0.3 | Photo. 3 months after AM transplant. Vision = 0.5 | |
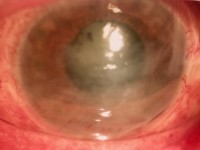
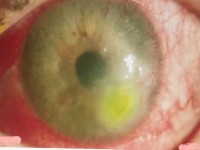
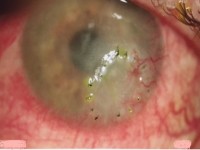
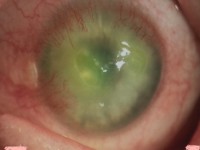
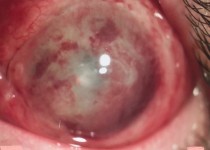
Clinical case 2: Patient B., 58 years old. Viral herpetic keratouveitis. Peripheral ulcer of the cornea. Transplantation of the amniotic membrane was performed on the left eye using the one-layer transplantation technique.
Photo OS. Erosion of the cornea, infiltration and edema of the stroma. Vision = 0.02 |
Photo OS. 1 day after AM transplant |
Photo OS. 1 month after AM transplant |
Photo OS. 3 months after AM transplant. Vision = 0.7 |
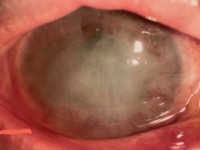
Clinical case 3: Patient P., 61 years old. Recurrent herpetic keratitis. Ulcer of the cornea. Transplantation of the amniotic membrane was performed on the left eye using the onlay technique of biological coverage.
Photo OS. Corneal erosion, infiltration and edema of the stroma. Vision = 0.01 |
Photo OS. 1 day after AM transplant |
Photo OS. 1 month after AM transplant |
Photo OS. 3 months after AM transplant. Vision = 0.1 |