Jesteś tutaj
Placenta Donation is Organ Donation
 The placenta is considered to be an organ1. It is one of the most remarkable human organs, because it is only designed to survive over the course of pregnancy. The placenta’s purpose is to support and protect the baby in the womb. The mother and the baby have separate blood supplies, and the placenta enables the migration of nutrition and oxygen from the mother’s blood to the baby’s blood. Also important, the placenta mediates between their immune systems, so that the mother’s immune system does not recognize the baby as foreign and attack the baby with antibodies.
The placenta is considered to be an organ1. It is one of the most remarkable human organs, because it is only designed to survive over the course of pregnancy. The placenta’s purpose is to support and protect the baby in the womb. The mother and the baby have separate blood supplies, and the placenta enables the migration of nutrition and oxygen from the mother’s blood to the baby’s blood. Also important, the placenta mediates between their immune systems, so that the mother’s immune system does not recognize the baby as foreign and attack the baby with antibodies.
Many people reading this article may have a little “organ donor” symbol on their driver’s license, signaling that in the event of death they want to donate their organs, tissues, and eyes. Our society has a very positive attitude towards organ donation; most people consider it a gift to save or enhance lives. Some countries have passed laws ruling that organ donation is the presumed choice upon death, unless the individual opts out2.
But some recent media reports have demonized placenta donations3,4. They have told the story of a mother giving consent on the operating table, they have assumed that the donations are funneled to unregulated stem cell clinics, and they have implied that it is wrong for procurement organizations to make money from tissue that was donated for free. Let’s take a deeper look at the similarities and differences between placenta donation and organ donation.
In the United States, we have a network of regional “Organ Procurement Organizations” (OPOs) that collect organs, tissues, and eyes from deceased donors5. We also have a national organization named United Network for Organ Sharing (UNOS) that assigns transplantable organs to patients on the waiting list6. As a result of this network, 2018 was the 6th consecutive year in which organ transplants broke previous records: there were 145 million adults registered to donate, there were over 113,000 patients on the wait list, donations were made by 10,722 deceased donors and 6,831 living donors, but over 5,800 patients on the wait list died6. In 2019 there has been a court battle over changes to the rules of organ allocation, changes that hopefully will save more lives, but will also cause financial losses to some transplant hospitals7.
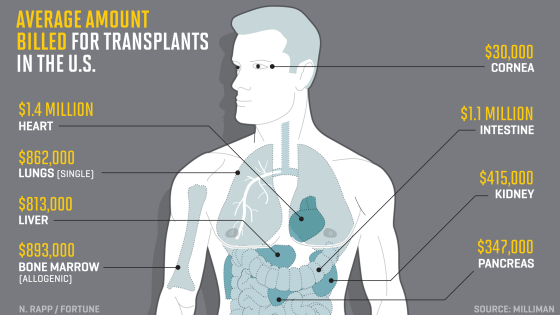 It is well known that organ transplants are very expensive, in terms of charges billed by the hospital to the patient’s insurance. The accompanying graphic shows the average charge per type of transplant, based on 2017 data researched by Milliman8 and presented in Fortune9. Some of the billed charges go to reimburse the OPO that provided the organ(s).
It is well known that organ transplants are very expensive, in terms of charges billed by the hospital to the patient’s insurance. The accompanying graphic shows the average charge per type of transplant, based on 2017 data researched by Milliman8 and presented in Fortune9. Some of the billed charges go to reimburse the OPO that provided the organ(s).
At present, there are over 50 OPOs operating in the United States that are accredited by the agency AOPO5. Parent’s Guide to Cord Blood Foundation looked up the most recently filed IRS financials for 43 of these OPOs that are registered as non-profits. Their annual revenue ranged from $5.4 to $376 million, and averaged $47 million. The assets of these OPOs averaged $46 million. It requires highly trained staff and advanced laboratory facilities to operate a successful OPO, which justifies the big budgets of the most highly accredited organizations.
How does placenta donation compare to organ donation? We have prepared a table that compares the steps to each process, and demonstrates that medically they are very similar. Parent’s Guide to Cord Blood Foundation is aware of at least 20 organizations that are collecting placenta donations in the United States. We were not able to summarize their financials, because most of them are subsidiaries of larger organizations: either they are part of a pharma company that develops products from the placenta, or they are a program at one of the non-profit OPOs that we have already described.
Procurement | Placenta Donation | Organs, Tissues, & Eyes from Deceased Donors |
Timing of Consent | Mother should not be in labor or under the influence of medication15 | Either donor registered before death or immediate family member gives consent15 |
Alternative fate of the organ | Discarded as medical waste. | Disposed by donor family. |
Checks on donor health | Questionnaire & Maternal blood test15 | Questionnaire if possible & Donor blood test15 |
Testing of the organ | Checked for diseases & external sterility15 | Checked for diseases & external sterility15 |
Handling and processing | Laboratory meets cGMP standards. | Organs tested in hospital. Tissues and eyes go to laboratory that meets cGMP standards. |
Time window from recovery to produce viable product | Within 48 hours | Some organs must be transplanted within a few hours. |
Medical products | Amniotic membrane, tissue matrix, tissue fragments. Cells that are Mesenchymal, Epithelial, Endothelial. Various combinations of the above. | Transplantable organs & corneas. Grafts of bone, tendons, and ligaments. Stem cells from bone marrow. |
Product applications that are already standard of care | Eye diseases and surgery. Wound dressings. Nerve wraps. Dental implants. Enhanced surgical recovery. Scar prevention. | Transplants of organs & corneas. Grafts of bone, tendons, ligaments. |
Research to increase clinical applications | Trials16 of perinatal stem cells for auto-immune diseases, neurologic disorders, and orthopedic procedures, among others. | Organ perfusion17,18 to keep the organ viable longer. Transplants19 that combine the organ with stem cells from donor bone marrow to decrease rejection. |
Examples of financial value | Public banks charge $36K to release donated cord blood13. The estimated value of a placenta is $50K14. | Health insurance companies pay8,9 $1.4M for heart transplant, $893K bone marrow transplant, $415K kidney, etc. |
Lives impacted in USA | Potential use: diabetic foot ulcers20-22 about 1 million per year; corneal ulcers23-25 about 34,000 per year. | 10,722 deceased donor organ transplants6 in 2018, over 1.5 million musculoskeletal allografts26 per year. |
In a recent article about placenta donation titled, The Afterlife of the Afterbirth, a bioethicist at the University of Minnesota told MedPage Today4: "What if women were given the full account, that some biobank is going to acquire it, process it, assign it value, and then it's going to be marked up and sold again…. Some women might think twice."
As part of informed consent, mothers giving birth should receive a full account of how their placenta donation might be used. It is illegal for the mother or her healthcare provider to be offered any financial incentive to donate. Accreditation standards require that the mother should not be in active labor or under the influence of drugs at the time of informed consent15. But it is unreasonable to expect that a biobank can acquire a donation, process it, and release it for patients without charging for their services. That is how procurement organizations stay in business and make it possible for patients to receive transplants and grafts of donated tissue.
The OPO industry used to have a problem with the perception that donated body parts get “marked up and sold again”. Back in 2012 the website MedicalTranscription.net provided data for an Infographic about organ values that was titled You Are Worth More Dead Than Alive10. Since it first appeared on the internet, this graphic has been reproduced and quoted in the media countless times. The OPO industry overcame that negative perception by producing lots of educational materials that emphasized the lives saved and the patient benefits realized from organ donations. For example, we have embedded an animated video from the US government promoting organ donation that was uploaded in Sept 201911. Nowhere over the course of this 5 minute video is anything shown about the finances involved. The entire focus is on saving lives.
This is the bottom line throughout the industries that process medical donations. It costs a lot of money to test and prepare donations for patients, and in the end the supplier must be reimbursed. When the Red Cross delivers blood transfusions to a hospital, they are paid for the product12. When Be The Match releases donated cord blood for a transplant, they get paid13. When OPOs provide organs for transplant, they get paid5-10. And yes, when companies provide products made from donated placentas, they are also paid14.
Placenta donation deserves the same respect accorded to donations of organs, tissues, and eyes. There are numerous medical products manufactured from placentas that are routinely used in FDA-approved treatments and clinical trials (see the table). The birth tissue industry has to push back against the media perception that placenta donation is a scam perpetuated on mothers at a vulnerable time. They need to produce more educational materials about how patients are helped by the donations, and stress their adherence to quality guidelines around informed consent and handling of tissues. Through improved public education, hopefully placenta donation will come to be regarded in the same positive light as organ donation.
DOWNLOAD this article as a pdf file.
References
- Loke YW. Life’s Vital Link: The Astonishing Role of the Placenta Oxford University Press 2013; ISBN: 978-0199694518
- Willis BH, Quigley M. Opt-out organ donation: on evidence and public policy. J R Soc Med. 2014; 107(2): 56–60.
- Chen C. The Birth-Tissue Profiteers. 7 May 2019. ProPublica
- Fiore K. The Afterlife of Afterbirth - Placenta donations may be feeding stem-cell scams. 15 Oct. 2019. MedPage Today
- Association of Organ Procurement Organizations (AOPO)
- United Network for Organ Sharing (UNOS)
- Farmer B. As Thousands Wait For Transplants, Medical Centers Fight To Keep Livers Close To Home. 14 May 2019. NPR All Things Considered
- Bentley TS, Phillips SJ. 2017 U.S. organ and tissue transplant cost estimates and discussion. 3 August 2017. Milliman Research Report
- Rapp N, VanderMey A. Here’s What Every Organ in the Body Would Cost to Transplant. 14 Sept. 2017. Fortune
- You Are Worth More Dead Than Alive. MedicalTranscription.net 2012. [Infographic]
- OrganDonor.gov (U.S. Government Information on Organ Donation and Transplantation) Organ Donation and Transplantation: How Does it Work? 2019. [Video]
- American Red Cross. What happens to donated blood? 2019. [Video]
- Kapinos KA, Briscombe B, Gracner T, Strong A, Whaley C, Hoch E, Hlavka JP, Case SR, Chen PG. Challenges to the Sustainability of the U.S. Public Cord Blood System. 29 Sept. 2017. RAND Research Report
- Schweizer R. What is your Placenta Worth? 2019; Parent’s Guide to Cord Blood Foundation. March 2019 newsletter
- American Association of Tissue Banks (AATB) Guidance Documents
- Couto PS, Bersenev A, Verter F. The first decade of advanced cell therapy clinical trials using perinatal cells (2005–2015). Regenerative Medicine 2017; 12(8):953-968
- Pan X, Yang J, Fu S, Zhao H. Application of ex vivo lung perfusion (EVLP) in lung transplantation. J Thorac Dis. 2018; 10(7):4637-4642.
- Ex Vivo Lung Perfusion (EVLP) - webpage for patients from Penn Medicine
- Leventhal J, Abecassis M, Miller J, Gallon L, Ravindra K, Tollerud DJ, King B, Elliott MJ, Herzig G, Herzig R, Ildstad ST. Chimerism and Tolerance Without GVHD or Engraftment Syndrome in HLA-Mismatched Combined Kidney and Hematopoietic Stem Cell Transplantation. Science Translational Medicine 2012; 4(124):124ra28
- American Diabetes Association (ADA) Statistics About Diabetes
- DiabeticFootOnline - 1 Day with #Diabetes in USA: Every 1.2 seconds someone develops a diabetic foot ulcer (DFU). From the Southwestern Academic Limb Salvage Alliance (SALSA). 2017.
- Armstrong DG, Boulton AJM, Bus SA. Diabetic Foot Ulcers and Their Recurrence. NEJM 2017; 376:2367-2375
- Holt Y. Amniotic Membrane uses in Ophthalmology. Parent’s Guide to Cord Blood Foundation. September 2017 newsletter
- Cason JB. Amniotic Membrane Transplant. American Association of Ophthalmology. 19 August 2019. EyeWiki
- Chang DC & Fusarium Keratitis Investigation Team. Multistate Outbreak of Fusarium Keratitis Associated With Use of a Contact Lens Solution. (34M people wear contacts USA, incidence microbial keratitis 5-21 per 10,000). JAMA. 2006; 296(8):953-963.
- Giedraitis A, Arnoczky SP, Bedi A. Allografts in Soft Tissue Reconstructive Procedures. Sports Health. 2014; 6(3):256–264.


