Usted está aquí
Timing of Cord Clamping: A critical issue for major medical centers

Recently, Parent’s Guide to Cord Blood Foundation released a brochure on the time of clamping of the umbilical cord after the birth of the baby. This brochure is given to pregnant women and suggests clamping in the range of 30-60 seconds (quoting American College of Obstetrics Gynecology or ACOG) for full term babies.
Since the early beginning of cord blood banking there has been controversy over the appropriate time of clamping the umbilical cord after the birth of the infant. Some believed the cord should only be clamped after it stops pulsating (which can take 3 minutes), so that the maximum amount of cord blood stem cells will enter the baby. Some believed the cord should be clamped immediately (within seconds of birth), to maximize the amount of cord blood stem cells that can be collected for future transplantation. The current recommendation to clamp at 30-60 seconds is a compromise between these extremes.
The author believes that clamping the cord while blood is returning to the infant, whether it is immediate or after a delay, is both medically and morally wrong. This method takes blood away from the infant. There is a concern that it could have a long-term unknown negative effect on the infant donor. For eons of time, this blood has gone back into the baby.
From the early 1990’s until recently, major medical centers performed cord blood collection after short clamping delays. These institutions should have records of the babies from which the cord blood was collected with either immediate clamping or 30-60 seconds clamping. It is their moral and medical responsibility to review these records and investigate what has happened to these infant donors. Did they develop diabetes, autism, etc.? It is incumbent on these medical institutions to review the health history of these donors and conduct a retrospective analysis for any morbidity that correlates with early clamping. It has been over 25 years since those infants had early clamping and this may not be long-term, but could be indicative a trend in morbidity.
The author believes this is an emergency situation. It is incumbent on the medical institutions that delivered babies with early cord clamping to review their records and attempt to evaluate the long-term health impact of their cord clamping delay times.
References
- Karl Rhodes. University of Richmond Magazine. Joined at the Cord. Winter 2005
- Ende M. Lymphangiosarcoma. Report of A Case Pac. Med. & Surg. 1966; (March-April):80-82
- Ende M. & Ende N. Hematopoietic Transplantation By Means Of Fetal (Cord) Blood. A New Method. Virginia Medical Monthly 1972; 99(3):276-80
- Ende N. The Berashis cell: a review--is it similar to the embryonic stem cell? Journal of Medicine. 2000; 31(3-4):113-30.
- Obituary of Milton Ende. Published in The Progress-Index June 29, 2007.
- Ende N, Weinstein F, Chen R, Ende M. Human umbilical cord blood effect on sod mice (amyotrophic lateral sclerosis). Life Sciences 2000; 67(1):53-59
- Ende N, Chen R. Human umbilical cord blood cells ameliorate Huntington's disease in transgenic mice. Journal of Medicine 2001; 32(3-4):231-240
- Ende N, Chen R, Ende-Harris D. Human umbilical cord blood cells ameliorate Alzheimer's disease in transgenic mice. Journal of Medicine 2001; 32(3-4):241-247
- Ende N, Chen R, Mack R. NOD/LtJ type I diabetes in mice and the effect of stem cells (Berashis) derived from human umbilical cord blood. Journal of Medicine 2002; 33(1-4):181-187
- Ende N, Chen R, Reddi AS. Transplantation of human umbilical cord blood cells improves glycemia and glomerular hypertrophy in type 2 diabetic mice. Biochemical and Biophysical Research Communications. 2004; 321(1):168-171
- Mi D, Fang H, Zhao Y, Zhong L. Birth weight and type 2 diabetes: A meta-analysis. Exp Ther Med. 2017; 14(6): 5313–5320.
- Ende N. & Reddi AS. Administration of human umbilical cord blood to low birth weight infants may prevent the subsequent development of type 2 diabetes. Medical Hypotheses 2006; 66(6):1157-1160



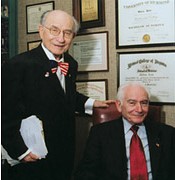 Brothers Milton and Norman Ende both went to medical school at the Medical College of Virginia in Richmond1. In 1966 Dr. Milton Ende pioneered the first published case of cord blood as a therapy for cancer2. In 1972 both brothers published the first attempt to give a cord blood transplant to a cancer patient3. The Ende brothers are often overlooked in official histories of cord blood transplantation because they did not use immune suppression before treating patients with cord blood, yet their publications demonstrated transient efficacy of cord blood alone. They called the stem cells in cord blood “Berashis” cells, after the Hebrew word for “Genesis”4. Dr. Milton Ende spent most of his career as a primary care doctor in Petersburg Virginia5, while Dr. Norman Ende was a pathologist on the faculty of the University of Medicine and Dentistry of New Jersey (UMDNJ). Dr. Norman Ende and colleagues performed a series of studies that examined how cord blood infusions altered the course of various disease models in mice6-8. Several papers explored the effects of cord blood infusions on mouse models of Type 1 and Type 2 diabetes9,10. Dr. Norman Ende and UMDNJ faculty member Alluru Reddi, PhD MD, a nephrologist who specializes in the treatment of diabetic microvascular complications, hypothesized that cord blood transfusions might protect low birth weight newborns from the development of type 2 diabetes later in life11,12. Dr. Norman Ende is now 94 years old and mostly retired, but he still actively follows news related to potential applications of cord blood. A full list of his publications can be found on his website,
Brothers Milton and Norman Ende both went to medical school at the Medical College of Virginia in Richmond1. In 1966 Dr. Milton Ende pioneered the first published case of cord blood as a therapy for cancer2. In 1972 both brothers published the first attempt to give a cord blood transplant to a cancer patient3. The Ende brothers are often overlooked in official histories of cord blood transplantation because they did not use immune suppression before treating patients with cord blood, yet their publications demonstrated transient efficacy of cord blood alone. They called the stem cells in cord blood “Berashis” cells, after the Hebrew word for “Genesis”4. Dr. Milton Ende spent most of his career as a primary care doctor in Petersburg Virginia5, while Dr. Norman Ende was a pathologist on the faculty of the University of Medicine and Dentistry of New Jersey (UMDNJ). Dr. Norman Ende and colleagues performed a series of studies that examined how cord blood infusions altered the course of various disease models in mice6-8. Several papers explored the effects of cord blood infusions on mouse models of Type 1 and Type 2 diabetes9,10. Dr. Norman Ende and UMDNJ faculty member Alluru Reddi, PhD MD, a nephrologist who specializes in the treatment of diabetic microvascular complications, hypothesized that cord blood transfusions might protect low birth weight newborns from the development of type 2 diabetes later in life11,12. Dr. Norman Ende is now 94 years old and mostly retired, but he still actively follows news related to potential applications of cord blood. A full list of his publications can be found on his website,