Sie sind hier
Options for Pain Control During Labor & Delivery
This is another in our series of interviews with Labor and Delivery nurse Kim Petrella, who is an advisor to Parent’s Guide to Cord Blood Foundation. After decades of experience delivering thousands of babies and educating other labor and delivery staff, Kim is our go-to resource for questions about childbirth.
An expectant mom’s options for pain control depend on a variety of factors. Contrary to popular belief, the amount of pain you’re in is NOT determined by how far your cervix has dilated. Some women have very hard and intense contractions when they are dilated 2 cm, while other women may be dilated 5cm and barely feeling their contractions. Labor can be divided into three phases, based on the strength and frequency of the contractions that are aiding your cervical dilation. Labor does not follow a script, and each mom is unique. This is why strategies to manage pain that work for one person may not work for another. Pain control during labor must be geared to each individual: her choices, her situation, and her laboring experience.
- Early Labor – (latent phase) – Contractions during this phase may be similar to menstrual cramps that you feel first in your back and thighs and then your abdomen. The contractions can be uncomfortable, but they are doing their part to “ripen” the cervix so that it is ready for delivery. Cervical ripening, also known as effacement, means that the cervix becomes thinner, shorter, and more dilated. Most of the time, you can spend this phase of labor at home. If you are at the hospital being induced, this phase of labor is usually the longest because the uterus is not contracting regularly yet.
- Mid Labor – (active phase) – During active labor your contractions become stronger, more regular, and progressively get closer together. If this is your first baby, your healthcare provider will want to talk to you (not your partner) on the phone. Most doctors will have you head into the hospital when you have contractions where you have to stop talking and breathe through them, they are 5 minutes apart, and this has been consistent for an hour. For a mom that has given birth before, your doctor may want you to head to the hospital sooner. Please call your provider before you head in to the hospital, so they can notify the nursing staff of your impending arrival and gather your records.
- Late Labor – (transition phase) – This is the most intense but shortest phase of labor for most women. In late labor, the cervix becomes fully dilated and mom may start feeling the urge to push the baby out. This is also the most painful part of labor.
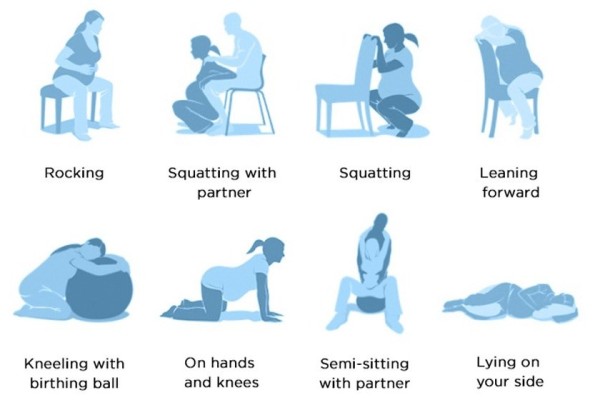
Movement is the best way to control pain during early labor, and the best way to help it progress. When mom keeps active, it helps to keep her muscles loose, and helps the baby to move into the correct position to come down the birth canal. “Movement” can be walking around the hospital unit or walking around the block, bouncing on a yoga ball, or dancing to your favorite music (Kim’s favorite). Almost any type of activity is good. Movement gives a sense of power and control over the pain during the early phase of labor.
It is important for Mom’s designated birth partner to be on hand right from the beginning of labor. It helps Mom to hear positive affirmations when she is going through such hard work. There are many ways that a birth partner or doula can help, such as timing rhythmic breathing, providing drinks and nutritious snacks, providing massage, or giving counter-pressure. The birth partner can take care of all the little things that go into maintaining a calm and positive atmosphere, such as keeping down the lighting and surrounding mom with aromatherapy.
Mid labor is where different moms will take diverging paths on how much pain control they desire. Pain control options have trade-offs, because certain forms of pain control will place restrictions on your ability to move around. On the flip side, pain control can be very welcomed assist for those moms that want a more controlled birth experience, or moms that are exhausted and need to take a break. Birth plans do change mid-labor all the time, so be open and flexible about what type of pain management you may need, and advise your birth partner to also keep an open and flexible attitude.
Today, many parents opt to watch videos online instead of attending hospital-based childbirth classes3. The disadvantage of this is that couples may not spend enough time together practicing the breathing techniques and positions that come in handy during labor. Effective labor partnering requires communication and practice. Start by talking regularly to your birth partner about your wishes and what you would like to have in your birth plan. Your birth partner is your advocate and may be able to talk to nurses and providers for you when you are unable to speak for yourself during contractions. Try to set aside time during your pregnancy to regularly practice some of the positions for relaxation, positions for pushing, and especially the rhythmic relaxation breathing. Do not practice pushing at home, but you can try the positions. Kim finds that when mom and her birth partner practice beforehand, they work together better during labor.
The following is a list of common options for pain control during mid-labor. No matter how much support mom is getting from her team, she is the one who is feeling the pain, and she is the one who has the final say on how much pain control she feels she needs.
- Natural, Unmedicated Birth – This is where teamwork and practice beforehand is a must! Labor and delivery are the Olympics of sports and the practice will be worth every second you put into it. Your labor nurse and/or midwife will help you, but they can’t be with you as much as your birth partner or doula. Be sure to educate yourself from sources that are reliable and trust-worthy and are not unrealistic.
- Nitrous Oxide – “Laughing gas” can be a pain relief bridge that will help mom to get farther along before requesting stronger pain control. Nitrous oxide is “self-administered”, which means mom holds a mask over her mouth and inhales as much or as little as she wants. Nitrous-oxide will usually not give you the giggles, but it provides a relaxed feeling and blocks pain signals to the brain4. It takes effect very quickly and wears off very quickly. The biggest advantage of this form of pain control is that it allows mom to keep walking. Check with your hospital in advance to see if they offer this method of pain control, since not all hospitals have this available.
- Narcotics – Intravenous pain medication will provide stronger relief that can help a mom experiencing powerful contractions to get back a feeling of control. Once mom receives an IV narcotic, she cannot walk around for a while, but she can still change positions on a bed. Narcotic pain control can be a great tool for someone who desires a minimally medicated birth, but needs a little help getting through a rough period or a prolonged labor. It can also help during the labor time before an epidural.
- Epidural anesthesia – The phrase “epidural” refers to an injection of pain killer into the epidural space around the spinal cord5-7. A trained anesthesiologist will insert a very thin catheter into this space which will deliver a continuous flow of numbing medication. The epidural catheter is taped securely to your back. It takes 15-30 minutes for the epidural to fully take effect. Once the epidural takes effect, you will be numb from your high waist down through your legs. An epidural relieves most of the pain from the contractions, but mom can still feel the pressure of the contractions during the pushing phase, so that pushes can be effective. Because you can’t feel your legs very well, walking around isn’t safe until your epidural medication wears off after your delivery. Mom needs to think about the timing of requesting the epidural, because if she is too close to birth it is no longer possible to keep still for the placement of the epidural and it is too late to wait for the epidural to take effect.
When can you get pain interventions?
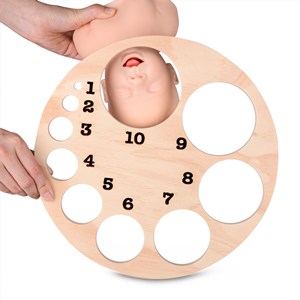 In the past, moms were told that they had to reach a certain number of centimeters of dilation before they could get an epidural. That rule has been discarded. The current policy of the American College of Obstetricians and Gynecologists (ACOG) is that a mom can get an epidural at any time during labor if she requests it7. That being said, moms are still encouraged to put the epidural off until they are fully in labor and not at risk of being sent home in early labor. It is also preferable to put off the epidural until mom can no longer tolerate moving around during labor.
In the past, moms were told that they had to reach a certain number of centimeters of dilation before they could get an epidural. That rule has been discarded. The current policy of the American College of Obstetricians and Gynecologists (ACOG) is that a mom can get an epidural at any time during labor if she requests it7. That being said, moms are still encouraged to put the epidural off until they are fully in labor and not at risk of being sent home in early labor. It is also preferable to put off the epidural until mom can no longer tolerate moving around during labor.
There is an old wives' tale that getting an epidural will slow down your labor, but research does not support this: “studies published since 2005 show no higher risk of assisted vaginal delivery with epidural than with opioid analgesia (as reported in a Cochrane review)”8. It should be noted that the dose of numbing medication used in epidurals today is lower than in the past, so mom will retain more ability to control her body, but the epidural can still dampen the ability to push hard. Your labor and delivery team at the hospital will assist you in finding the right muscles to push and getting you into positions that work with epidurals.
Monitoring during labor and pain control
Fetal monitoring needs to be discussed in the context of pain control, because the amount of monitoring that you need may influence your choices for pain control. The phrase “monitoring” the baby primarily means listening to the fetal heart rate while simultaneously timing contractions. Doctors and midwives can infer a great deal about how the baby is tolerating labor just by listening to the heart rate before, during, and after contractions.
 Some moms only need intermittent monitoring, whereas some moms will be requested to wear a continuous monitoring device. The standard monitoring system consists of two stretch belts: one belt holds a device to measure the fetal heart rate, and the other belt holds a device to measure the contractions9. Some hospitals offer monitors that send their measurements wirelessly, and this will allow mom to have a pretty full range of movement. But the wireless monitors are not as accurate as the ones with a wired connection, and your doctor may want you to wear a wired monitor to get a very clear picture of how the baby is responding to the contractions. Being attached to a wired monitor will restrict mom’s range of movement. There is even an option of internal monitoring, where the doctor reaches up to the cervix and gently attaches a wired probe to the baby’s head.
Some moms only need intermittent monitoring, whereas some moms will be requested to wear a continuous monitoring device. The standard monitoring system consists of two stretch belts: one belt holds a device to measure the fetal heart rate, and the other belt holds a device to measure the contractions9. Some hospitals offer monitors that send their measurements wirelessly, and this will allow mom to have a pretty full range of movement. But the wireless monitors are not as accurate as the ones with a wired connection, and your doctor may want you to wear a wired monitor to get a very clear picture of how the baby is responding to the contractions. Being attached to a wired monitor will restrict mom’s range of movement. There is even an option of internal monitoring, where the doctor reaches up to the cervix and gently attaches a wired probe to the baby’s head.
Another issue that comes up with fetal monitoring, is that mom may need to stay in a specific position which the baby tolerates better. Under these circumstances, mom may need more pain relief because movement and position changes are not an option. This is an example of how labor is an unscripted experience. You can go into labor with a birth plan, but if baby doesn’t cooperate, you may be forced off your plan.
By the time you make it to late labor, most likely you have already made a decision about how to manage pain control. Listen to your provider while pushing, because you may receive last-minute instructions to follow.
Before the baby arrives, make sure you have talked to your birth partner and your care team about your choices for the moments right after birth. You may be too tired after the birth to talk, so be sure to discuss your wishes in advance. Have you discussed the timing of delayed cord clamping? Does your partner want to cut the umbilical cord? Are you providing a kit for cord blood collection? Do you want to hold the baby on your chest with skin-to-skin contact? Would you like to try early breastfeeding? Do you have any cultural or spiritual desires for the birth? Be sure to include all these decisions in your birth plan and discuss them upon admission.
Kim says “expectations for labor may not always be met, but this should not be viewed as a disappointment”. The goal is to finish the delivery with a healthy baby and a healthy mom, no matter how you get there. A birth can be beautiful and exciting, but it can also be scary and fast, so remember to be open and flexible about how to manage the pain and any changes of plans. Once your baby is in your arms, no matter how they get there, it is one of life’s most beloved treasures! Be sure to be proud of yourself for getting to the finish line.
References
- Bellefonds C, Greenberg J. What Are the Stages of Labor and How Long Does Labor Last? What to Expect. Published 2021-09-07
- Lothian JA. Labor Day: What To Expect. Lamaze. Accessed 2025-10-01
- Teen L. Mommy Labor Nurse.
- Spencer C. 5 FAQ about laughing gas for pain relief during labor, delivery. Mayo Clinic. Published 2022-03-17
- Asher A, Olufade O. Epidural Space Anatomy and Injections. Verywell Health. Published 2025-06-07
- MacMillan C. Epidurals During Childbirth: What Women Should Know. Yale Medicine. Published 2023-03-16
- American College of Obstetricians & Gynecologists. Medications for Pain Relief During Labor and Delivery. FAQs for Patients. Last reviewed 2024-10
- Callahan EC, Lee W, Aleshi P, George RB. Modern labor epidural analgesia: implications for labor outcomes and maternal-fetal health. Am. J. Obstetrics and Gynecology. 2023; 228(5S):S1260-S1269.
- American College of Obstetricians & Gynecologists. Fetal Heart Rate Monitoring During Labor. FAQs for Patients. Last reviewed 2023-11