Jste zde
What is your Placenta Worth?
Parents should read our companion article, Can you sell your baby's placenta?
 Unique, to say the least
Unique, to say the least
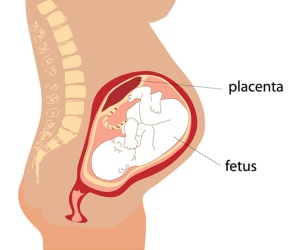
The placenta remains the least understood human organ. But thanks to organizations like The Centre For Trophoblast Research1, and scientists like Professor Y.W. Loke of Cambridge University2, we are beginning to understand the flawless organization and intricate performance of our placenta. For example, few people are aware that the placenta is derived from the baby. It becomes closely embedded in the mother’s womb such that the baby can “borrow” everything it needs to develop1. We are learning that many of the medical problems encountered later in life are a direct result of placenta dysfunction2. The hope is that a better understanding of the placenta will lead to broader knowledge in other critical areas of healthcare.
The Placenta’s 2nd Life
Your placenta can continue to provide therapeutic value and have a 2nd life if the afterbirth is not discarded as medical waste. Components isolated from the placenta, such as the umbilical cord blood, and the amniotic membrane, are already serving a valuable role in medicine today. Research continues to develop the therapeutic value of other components of the placenta. With our skills in cryopreservation, your placenta can be preserved for future applications in personalized medicine. The placenta’s 2nd life encompasses new treatments today and bio-banking for the future. We are rapidly moving into a new paradigm where the placenta is transitioning from biological waste to becoming a biological toolbox for cures.
Therapies for Today and Tomorrow
We consider the following to be the therapeutic components of the placenta, either today or tomorrow:
- Cord/Placental blood – Over 35,000 cord blood transplants have been performed worldwide3, with thousands more joining the list each year4. Cord blood transplants comprise living cells and are performed under FDA approval.
- Amniotic Membrane of the Placenta (AMP) – Both viable (living) and non-viable (freeze dried) AMP tissue products are used every day as skin substitutes for wound care. AMP products also have well-established applications in ophthalmology, orthopedics, gynecology and urology.
- Mesenchymal stem/stromal cells (MSC’s) can be derived from the tissue of the placenta, amnion, and chorion, as well as the Wharton’s Jelly that fills the body of the umbilical cord. There are currently about 150 new clinical trials each year that utilize MSC for regenerative medicine5, and perinatal tissues provide the largest percentage of MSC in clinical trials6.
- Epithelial stem cells are found in the amnion. They are precursors to growing skin and have cell markers similar to pluripotent stem cells.
- Endothelial cells – These are derived from the lining of blood vessels in the umbilical cord and are currently studied for applications in vascular diseases.
- Extracellular Matrix (ECM) of the placenta has value as a decellularized scaffold material for biological engineering.
- Chorion tissue – Like the AMP, chorion tissue isolated from the placental sac has been used whole in wound care products.
- Umbilical Cord Tissue – Thicker and stronger than AMP, this tissue can be used in surgical applications as an allograft or stent wrap.
- Conditioned Media – There are numerous beneficial factors that are secreted by perinatal cells and tissues, including cytokines, hyaluronic acid, growth factors, etc.
 The Placenta Paradigm Shift
The Placenta Paradigm Shift
As we become mindful of the placenta’s broader therapeutic future, organizations that collect birth tissues have become more ‘whole placenta’ minded. We need to isolate and utilize as much of the placenta as possible for research, clinical study, and current product fulfillment. However, distribution is typically fragmented, and many companies justifiably focus on only one type of product, so consequently there is waste. Also, the ability to successfully cryopreserve several of these components, such as ECM, is still in development.
Hype will always precede the commercialization of a breakthrough technology, and placenta-based products and therapies are no exception. Saving a life is certainly priceless and cannot be monetized, but today thousands of dollars in value are being attached to placenta donations. When we include our AmnioChor model of bio-banking for future use, the placenta becomes the gift that will keep on giving.
Placenta Valuation
We know that falsely marketed products and treatments are running rampant today and people are getting wealthy at the expense of the good name of the placenta. An accurate valuation of what your placenta is worth must include the following considerations:
- By AmnioChor's estimate, the AMP market, which is a significant contributor to placenta value today, will grow to over $600M in 2020. Although insurance reimbursement exists for many AMP products, at present these products are only sourced from donations of C-Section placentas.
- The price of placenta products is driven up by the multi-tiered structure of the procurement chain: One company collects birth tissues, a second company manufactures products, and a third delivers them as therapy.
- The laboratory processing of the placenta is highly variable right now, can be costly, and this will continue for quite some time as new methods and efficiencies are developed.
- Valuation of the placenta should contemplate both today and tomorrow products. The ability to bank placenta tissue and cells and derive multiple personalized therapies will drive the valuation higher, but the costs of tomorrow products are obviously not yet known.
- We are dealing with potentially lifesaving products in a market that today is largely an unregulated ‘what-the-market-will-bear’ environment. Tomorrow’s market will be more regulated and FDA compliance will lead to higher product costs.
- As therapeutic benefits are realized, we believe that more placenta products will be covered by insurance reimbursement, and this will drive a leveling of the valuations.
- With any new technology there is great value fluctuation as the industry strives to achieve economy of scale and cost effectiveness. Hence we caution against runaway inflation of placenta valuations.
A recent blog by Dr. Chris Centeno placed the value of all afterbirth products at over half a million dollars per birth7. However, the majority of that high valuation was driven by amniotic fluid, which we do not include here. Although research indicates that amniotic fluid can be collected on a large scale during C-section births and contains valuable cells, the cells are present at low concentrations compared to cells isolated from cord blood or perinatal tissues8.
 How to Incentivize Placenta Donors
How to Incentivize Placenta Donors
Donation is the backbone of life saving organ and stem cell transplants as well as regenerative medicine. To stifle that caring and sharing human dynamic would be catastrophic. As a society we have an ethical responsibility to both advance medical technology and to further grow donation networks to build the community transplant capacity that will save lives. Most people agree that providing mothers with an incentive to donate their placenta would be a good thing, if it is done in an ethical way.
We must be aware of The National Organ Transplant Act of 1984 (NOTA)9-11. NOTA made it illegal to compensate organ donors, but did not prevent payment for other forms of donations, such as blood, sperm, and eggs. Since the placenta is considered an organ, now and for the foreseeable future, financial compensation for placenta donation is illegal and carries stiff punishment for violation.
In lieu of financial compensation, some have suggested that donating mothers should receive a gift or service12. A better option is to give the donating mother something of substantial future value: storage of her child’s stem cells. What if we provide donors with a level of private banking at little to no cost? As a business there is an opportunity to leverage two capabilities: both donation for product development as well as personal storage for the family, and this can be done for multiple cell lineages found in the placenta and umbilical cord. When we achieve launch, AmnioChor will offer an Omnibank that operates on the philosophy to “leave no cell behind”.
References
- Centre for Trophoblast Research
- Loke YW. Life’s Vital Link: The Astonishing Role of the Placenta Oxford University Press 2013; ISBN: 978-0199694518
- Ballen KK, Verter F, Kurtzberg J. Umbilical cord blood donation: public or private? Bone Marrow Transplantation 2015; 50:1271–1278
- World Marrow Donor Assocation
- CellTrials.org blog 31 March 2018: Counting Keywords is not Compiling Clinical Trials: Mesenchymal
- CellTrials.org data package: MSC Trials 2011-2018
- Centeno C. Regenexx blog 25 January 2019: What Are the Bioethics of Sourcing Birth Tissues and Selling Them for Huge Money?
- Moraghebi R, Kirkeby A, Chaves P, et al. Term amniotic fluid: an unexploited reserve of mesenchymal stromal cells for reprogramming and potential cell therapy applications Stem Cell Research & Therapy 2017; 8:190
- NIH Legislative History: National Organ Transplant Act
- National Living Donor Assistance Center: National Organ Transplant Act
- Wikipedia: National Organ Transplant Act of 1984
- Medium Magazine 25 July 2018: Should We Pay Mothers to Donate Placentas?