Jste zde
Collector Training Improves Cord Blood Collections

Parents anxiously expecting the arrival of their baby have a multitude of decisions to make. From "What color do I paint the nursery?" to "Do I try natural childbirth?". While parents have been grappling with these questions for decades, a relatively new question has arisen: "Do I donate or save my baby's cord blood?"
Private cord blood banks inundate expectant parents with marketing literature and advertisements concerning the benefits of privately banking a baby's cord blood. Public cord blood banks that seek donations to help patients tend to have more modest marketing budgets, if any budget at all. Whereas private banking costs parents over a thousand dollars in the first year, public donation is free.
Approximately 70% of patients who need a stem cell transplant do not have a match within their family, so that registries of adult donors and cord blood donations are their only hope for a cure. Because the matching requirements are not as stringent for cord blood transplants as they are for transplants from adult donors, cord blood plays a vital role in offering access to a cure to all patients. Public cord blood banks currently make cord blood units available for use in stem cell transplants to cure a range of diseases from leukemia to lymphoma and a host of 60+ other genetic diseases found in children.
Public and private banks also differ in how they collect cord blood. Private banks rely solely on the mother's caregivers to collect the cord blood after the baby is born. Private collections may be performed by a medical doctor, a nurse, or a midwife. Public banks rely on a mix of doctors who received extra training in cord blood collection and dedicated cord blood collection specialists who work at the delivery hospital.
Our hospital, Brigham & Women's, is the largest birthing center in the state of Massachusetts, with nearly 8000 births a year. However, we cannot afford to employ cord blood collection specialists on a 24/7 basis, so we began training doctors to collect cord blood at those times when the staff are not available.
We compared the size of the cord blood collections performed by doctors versus those collected by the dedicated collection staff. The basic volume threshold for storage in a public bank is 80 mls. While ultimately cell dose is the deciding factor as to whether a collection is "bankable", volume is used as a surrogate marker. Cell dose refers to the number of stem cells in the cord blood prior to cryopreservation. There must be enough stem cells to engraft and create a new immune system for an adult-sized patient.
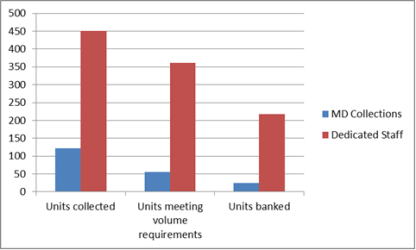
During 2012, a total of 998 mothers consented to donate. But 99 collections were not attempted because there was no trained staff available to perform the collection. A total of 899 collections were attempted. From those attempts, 573 total cord blood units were collected, but 151 of the collected units were too low in volume to ship for processing (26.3%). Among the remaining 422 cord blood units that were shipped to the bank, 56 were collected by doctors or midwives (13.3%) and 366 were collected by the Collection Specialist staff (86.7%). Ultimately, 48% of the 366 cord blood units collected by dedicated collection staff were banked, while only 20.5% of the 56 collections by medical staff were banked.
Our study shows that dedicated collection staff outperform medical staff in both the number of cord blood collections that exceed the volume threshold by a factor of 6.5, and in obtaining collections that pass all banking criteria by a factor of 15.3. These results should not reflect poorly on the doctors and other medical staff who take the time to participate in this process, but rather on the fact that the medical staff are there to take care of mom and baby and cord blood collection is a secondary thought. In addition, we can comment from our experience that your music teacher was right, "practice makes perfect". The more collections you perform, the better you are at collecting.